UnitedHealthcare Shared Services members can access our network
UnitedHealthcare Shared Services is a service model that gives plan sponsors access to the UnitedHealthcare network but allows them to self-administer plan benefits or have a third-party administrator (TPA) administer benefits on their behalf. This means you can treat members with UnitedHealthcare Shared Services because they have access to our network.
Member ID card
The following member ID card example shows you how to tell when a patient is a UnitedHealthcare Shared Services member.
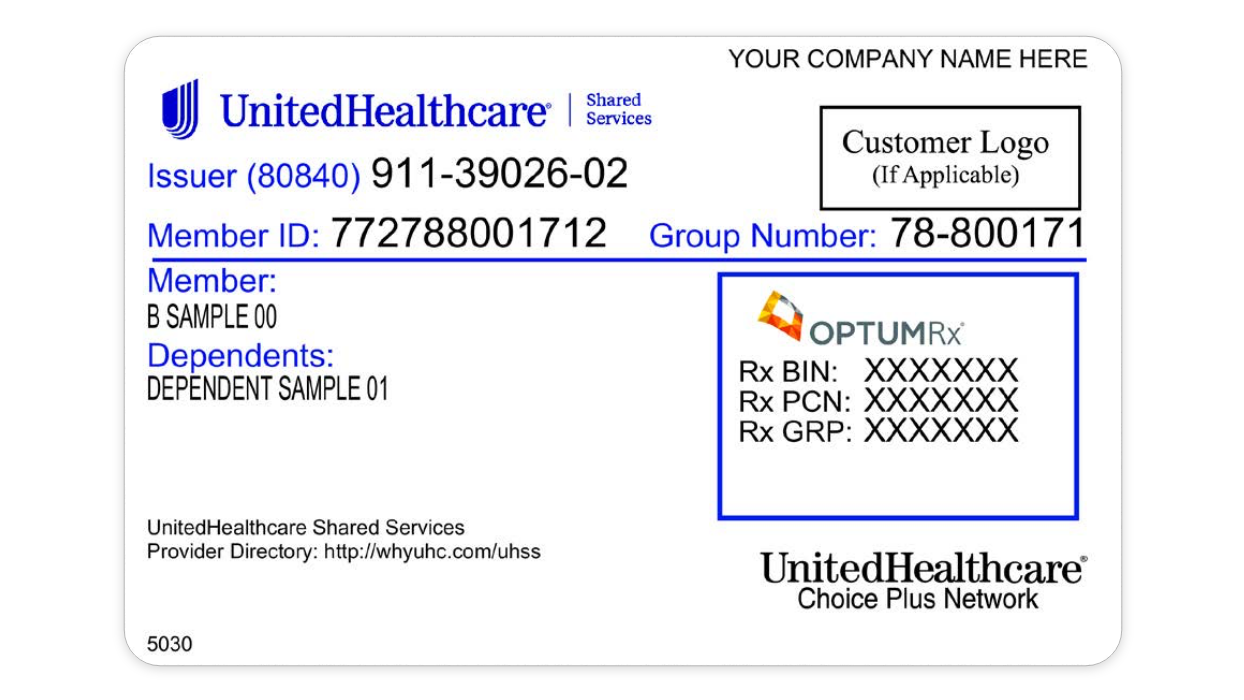
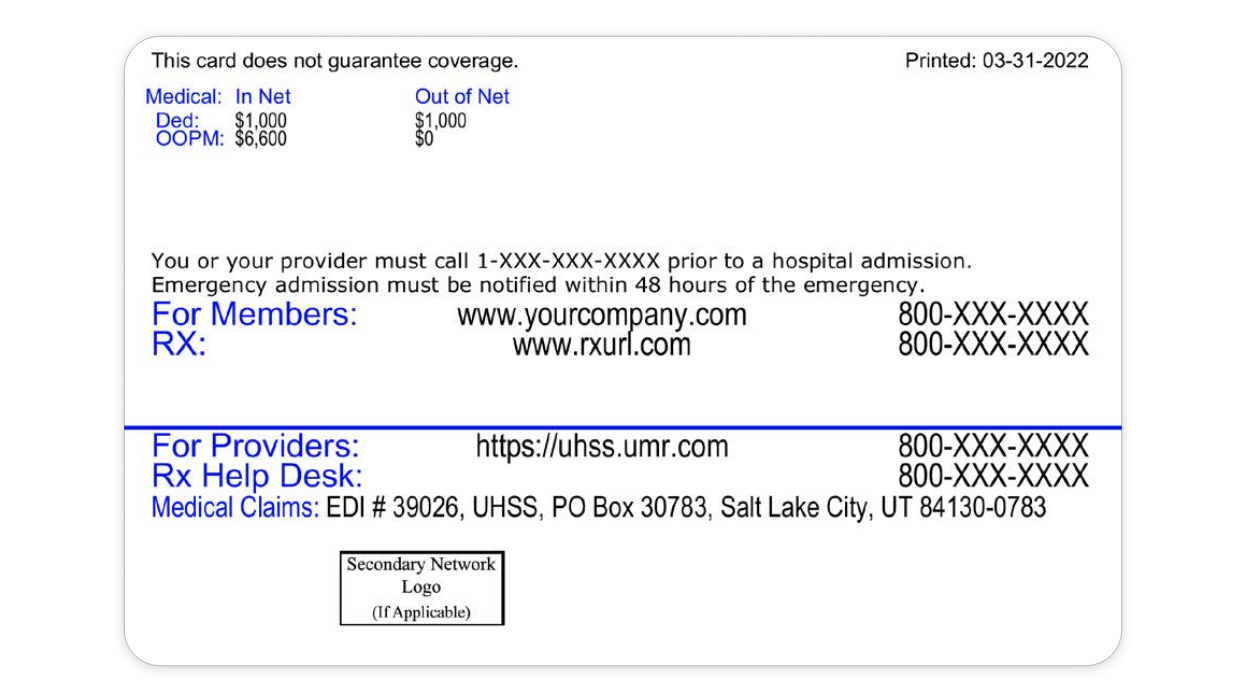
Sample member ID card for illustration only; actual information varies depending on payer, plan and other requirements
Checking eligibility, benefits and claim status
- Visit uhss.umr.com
- Call the Provider Services number on the back of the member’s ID card
Submitting prior authorizations
You must call the phone number on the back of the member ID card to submit prior authorizations. Prior authorizations for UnitedHealthcare Shared Services members can’t be submitted through the UnitedHealthcare Provider Portal.
Prior authorization and notification requirements are outlined in your UnitedHealthcare Administrative Guide, and some plans may have additional prior authorization requirements.
Learn more
- Visit the Find a Provider section on whyuhc.com/uhss to confirm you’re a participating provider
- View this interactive guide for more information on UnitedHealthcare Shared Services